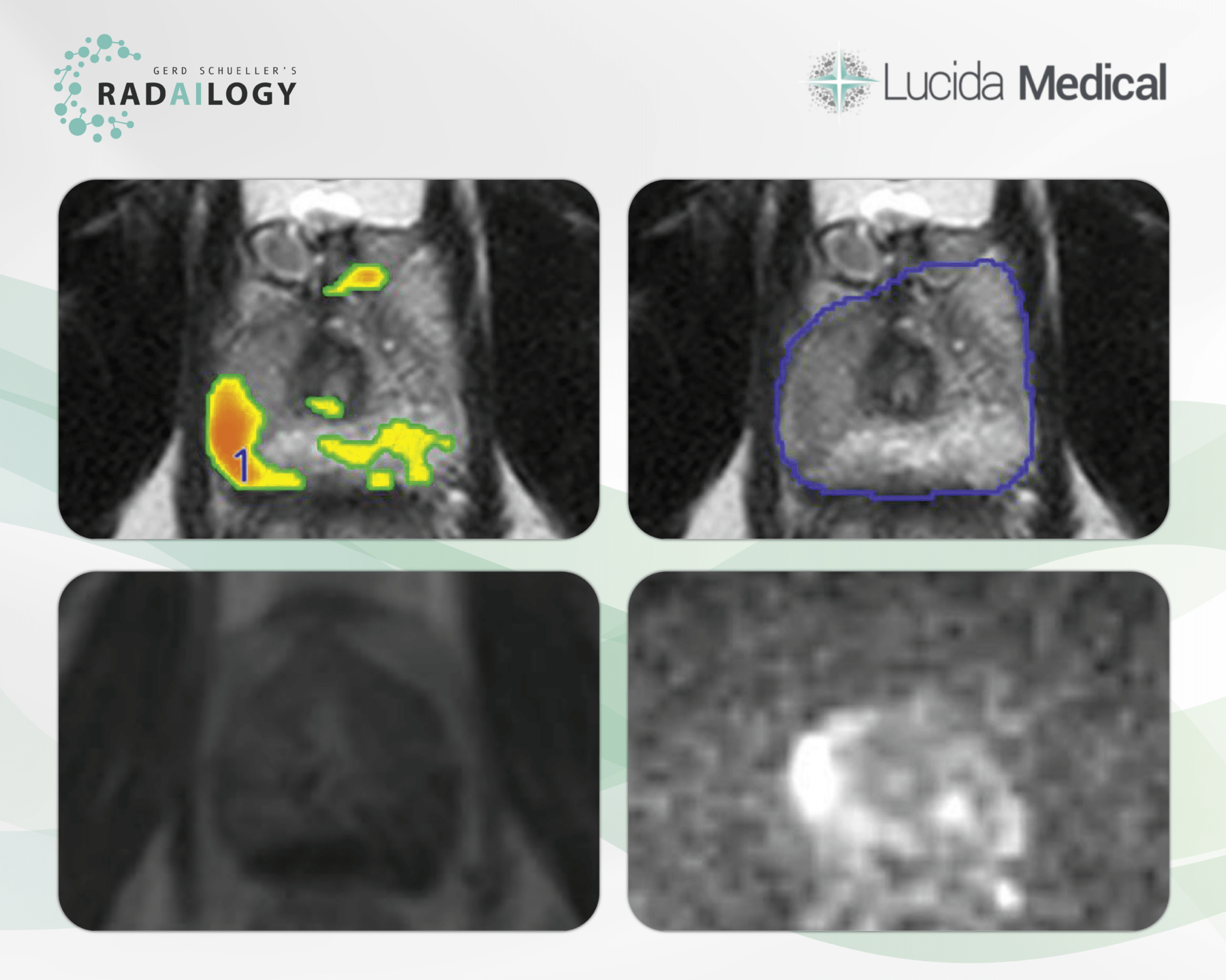
Axial T2 (upper left and right), contrast enhanced T1 (DCE, lower left) and DWI (lower right) MRI of the prostate of a 52-year-old patient with a Gleason Score of 4. T2 hypointensity in the middle peripheral zone on the right with corresponding hyperintense DWI signal and marked hypervascularization. Prostate Intelligence has detected (overlaid to T2 axial, upper left) and rated the lesion as AI-Likert 4.3. The AI assistant detected additional non suspicious nodular lesions in the central, transitional and left peripheral zones, respectively (overlaid to T2 axial, upper left). Prostate Intelligence quantified the prostate volume as 51 ml (not shown). Histopathology confirmed the lesion in the right peripheral zone malignant.
MRI of the prostate is an important area of oncological radiology. It takes years of radiological experience to distinguish malignant lesions from benign changes. Furthermore, prostate imaging is an excellent example of close collaboration between radiologists and clinicians. How should the MRI be evaluated in regard to the Gleason score? How stringent is the topographical depiction of the lesions? Which lesions are determined as biopsy targets?
It is with great pleasure that we present Prostate Intelligence, an AI assistant for the detection and analysis of prostate cancer in MR studies.
Why Prostate Intelligence matters and how it works
Prostate Intelligence helps detect and analyze prostate cancer in MR studies. The results are clearly structured with heat maps and tables and enable the selection of biopsy targets. The evaluation of the results is based on the PI-RADS classification. Prostate Intelligence helps radiologists and clinicians save time, particularly when it comes to organ and tumor segmentation. The interdisciplinary case discussions improve in quality.
Who benefits
Clinicians and radiologists through the detailed visualization and diagnosis of prostate cancer in comprehensive images.
Our own experience at Radailogy
Prostate Intelligence convinced us in many ways. The sensitivity, NPV and AUC are each reported as >90% at an AI score threshold of 3.5. According to the AI manufacturer, Lucida Medical, the specificity of at least 78% is only achieved with a Gleason score of 4. Our tests based on our own patient data even outperformed the manufacturer’s data with a Gleason score <4. We observed a high TN rate of >95%. The classification of prostate tumors is given as a five-point AI Likert scale and is based on the PI-RADS score. Prostate Intelligence automatically calculates the prostate volume. The segmentation work is also pleasingly detailed, saves time and provides precision for radiological diagnosis and knowledge transfer to clinicians and patients. Prostate Intelligence can be seamlessly integrated into your daily workflow.
Any medical professional can use Prostate Intelligence for each individual patient by quickly and easily uploading MRI studies of the prostate to Radailogy. Our telemedicine customers also use this AI assistant as a standard in daily practice to optimize their oncology workflow.
The scientific evidence
Sushentsev N, Moreira Da Silva N, Yeung M, Barrett T, Sala E, Roberts M, Rundo L. Comparative performance of fully-automated and semi-automated artificial intelligence methods for the detection of clinically significant prostate cancer on MRI: a systematic review. Insights Imaging. 2022 Mar;13(1):59
Data to upload to Radailogy
1.5-3.0 Tesla, imaging planes should be the same across T2, DWI and DCE; T2: recommended slice thickness 3mm, imaging resolution <0.65mm; DWI & ADC: TE ≤90 msec; TR ≥3000 msec, slice thickness ≤4mm, no gap, resolution ≤2.5mm phase and frequency, high b-value ideally 800-1000; Contrast enhanced T1 (DCE): TR/TE <100msec <5msec, slice thickness 3-4.5mm, no gap, resolution ≤2mm, post contrast total observation >2min. Ideally the enhancement peak should occur at least 1min before observations stop. There is no need for DCE observations longer than 3min.